Understanding Plaque Formation in Arteries
Arteries are vital blood vessels that transport oxygen-rich blood from the heart to various parts of the body. Maintaining their health is crucial for overall cardiovascular function. However, arteries can undergo a pathological process known as plaque formation, which can lead to serious health complications such as atherosclerosis, heart attacks, and strokes. Understanding how plaque forms, the factors that contribute to its development, and the ways to prevent and manage it is essential for maintaining heart health and preventing cardiovascular diseases.
To understand how plaque, risk factors, and prevention fit into the larger cardiovascular picture, read the cornerstone guide: Cardiovascular Health: The Definitive Guide to Heart and Vascular Wellness.
What is Arterial Plaque?
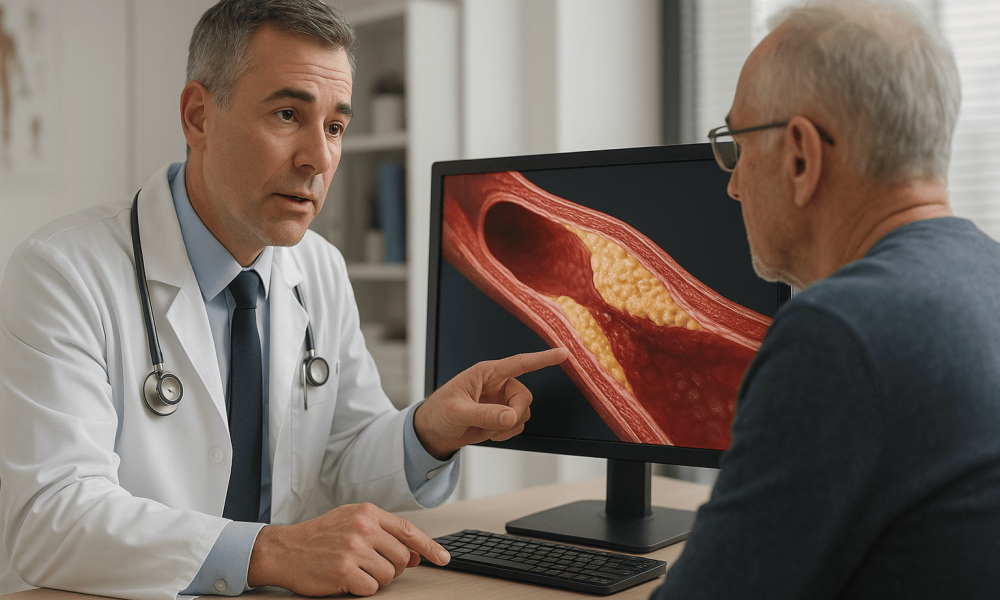
Arterial plaque, also known as atherosclerotic plaque, is a buildup of substances within the walls of arteries. This accumulation narrows and stiffens the arteries, restricting blood flow and oxygen delivery to vital organs. Over time, plaque can lead to the hardening of arteries, a condition known as atherosclerosis, which is a major risk factor for heart disease and stroke.
Composition of Arterial Plaque
Arterial plaque is composed of various substances, including:
- Cholesterol: Low-density lipoprotein (LDL) cholesterol is a primary component, contributing to plaque buildup.
- Fatty Acids: Saturated and trans fats can accumulate within arterial walls.
- Calcium: Deposits of calcium can harden the plaque, making arteries less flexible.
- Cellular Debris: Dead cells and other cellular waste products are incorporated into the plaque.
- Inflammatory Cells: Macrophages and other immune cells are involved in the inflammatory response associated with plaque formation.
The Process of Plaque Formation
Plaque formation in arteries is a gradual process that involves multiple stages. Understanding these stages helps in comprehending how cardiovascular diseases develop and progress.
Endothelial Dysfunction
The process begins with damage or dysfunction of the endothelium, the thin layer of cells lining the interior surface of blood vessels. Factors contributing to endothelial dysfunction include high blood pressure, smoking, high cholesterol levels, diabetes, and inflammation.
- High Blood Pressure: Excessive force against artery walls can damage the endothelium.
- Smoking: Toxins in cigarette smoke promote inflammation and oxidative stress.
- High Cholesterol: Elevated LDL cholesterol can penetrate the endothelial layer.
- Diabetes: High blood sugar levels can impair endothelial function.
LDL Cholesterol Accumulation
Once the endothelium is compromised, LDL cholesterol particles can infiltrate the arterial wall. These particles undergo oxidation, making them more reactive and inflammatory.
- Oxidized LDL: Oxidation changes the structure of LDL, making it more likely to be taken up by immune cells.
- Immune Response: The body recognizes oxidized LDL as foreign, triggering an immune response.
Inflammatory Response and Foam Cell Formation
Macrophages, a type of white blood cell, engulf the oxidized LDL particles, becoming foam cells. These foam cells accumulate within the arterial wall, contributing to the formation of fatty streaks, the earliest visible signs of atherosclerosis.
- Foam Cells: Macrophages filled with oxidized LDL become foam cells, which are a hallmark of early plaque development.
- Fatty Streaks: These are initial, non-obstructive plaques composed mainly of foam cells and lipids.
Progression to Fibrous Plaques
As the fatty streaks persist, smooth muscle cells migrate to the site and begin to produce extracellular matrix proteins, such as collagen. This leads to the formation of fibrous plaques, which are more stable and harder.
- Fibrous Cap: A layer of collagen and smooth muscle cells covers the lipid-rich core, stabilizing the plaque.
- Calcification: Over time, calcium deposits accumulate, further hardening the plaque and reducing arterial flexibility.
Plaque Rupture and Thrombosis
In some cases, fibrous plaques can become unstable and rupture. When a plaque ruptures, it exposes the underlying lipid core to the bloodstream, triggering the formation of a blood clot (thrombosis). This clot can significantly narrow or completely block the artery, leading to acute cardiovascular events such as heart attacks or strokes.
- Heart Attack: If a clot blocks a coronary artery, it can result in myocardial infarction, causing damage to the heart muscle.
- Stroke: A clot in a cerebral artery can disrupt blood flow to the brain, leading to ischemic stroke.
Risk Factors for Plaque Formation
Several factors increase the risk of plaque formation in arteries. Managing these risk factors is essential for preventing atherosclerosis and associated cardiovascular diseases.
High Cholesterol Levels
Elevated levels of LDL cholesterol and low levels of high-density lipoprotein (HDL) cholesterol contribute significantly to plaque buildup.
Hypertension (High Blood Pressure)
Consistently high blood pressure can damage the endothelium and promote plaque formation.
Smoking
Tobacco use accelerates the development of atherosclerosis by promoting inflammation and endothelial dysfunction.
Diabetes
High blood sugar levels associated with diabetes can damage blood vessels and increase the risk of plaque buildup.
Obesity
Excess body weight is linked to higher blood pressure, increased cholesterol levels, and insulin resistance, all of which contribute to atherosclerosis.
Physical Inactivity
Lack of regular exercise is associated with higher cholesterol levels, hypertension, and obesity, increasing the risk of plaque formation.
Unhealthy Diet
Dietary patterns high in saturated fats, trans fats, and cholesterol promote elevated LDL levels and contribute to atherosclerosis.
Family History
A family history of heart disease can predispose individuals to plaque formation and atherosclerosis.
Impact of Plaque Formation on Cardiovascular Health
The buildup of arterial plaque has profound effects on cardiovascular health, leading to various complications that can significantly impact an individual’s quality of life and longevity.
Coronary Artery Disease (CAD)
CAD occurs when plaque buildup narrows the coronary arteries, reducing blood flow to the heart muscle. This can lead to angina (chest pain) and, in severe cases, myocardial infarction (heart attack).
Peripheral Artery Disease (PAD)
Plaque accumulation in the peripheral arteries, particularly in the legs, can cause pain, numbness, and increased risk of infections due to reduced blood flow.
Carotid Artery Disease
Plaque in the carotid arteries can lead to reduced blood flow to the brain, increasing the risk of transient ischemic attacks (TIAs) and strokes.
Aortic Atherosclerosis
Plaque formation in the aorta can lead to aneurysms (abnormal bulges in the artery wall) and increase the risk of rupture, which is a life-threatening emergency.
Heart Failure
Chronic atherosclerosis can weaken the heart muscle over time, leading to heart failure, where the heart cannot pump blood effectively to meet the body’s needs.
Prevention of Arterial Plaque Formation
Preventing plaque formation involves adopting a heart-healthy lifestyle and managing underlying health conditions. These strategies can significantly reduce the risk of atherosclerosis and its associated complications.
Healthy Diet
Adopting a diet low in saturated fats, trans fats, and cholesterol can help maintain healthy cholesterol levels and prevent plaque buildup.
- Increase Intake of Fruits and Vegetables: Rich in fiber, vitamins, and antioxidants, these foods support overall heart health.
- Choose Whole Grains: Whole grains like oats, brown rice, and quinoa can help lower cholesterol levels.
- Opt for Lean Proteins: Incorporate sources such as poultry, fish, legumes, and nuts into your diet.
- Limit Processed Foods: Reduce consumption of processed and fast foods that are high in unhealthy fats and sodium.
- Use Healthy Fats: Replace saturated and trans fats with healthier options like olive oil, avocados, and fatty fish rich in omega-3 fatty acids.
Regular Physical Activity
Engaging in regular exercise strengthens the heart, improves blood circulation, helps maintain a healthy weight, and lowers blood pressure and cholesterol levels.
- Aerobic Exercise: Activities such as walking, jogging, cycling, and swimming for at least 150 minutes per week.
- Strength Training: Incorporating muscle-strengthening exercises at least two days a week.
- Flexibility and Balance: Practices like yoga and tai chi can enhance overall physical fitness and reduce stress.
Maintain a Healthy Weight
Achieving and maintaining a healthy body weight reduces the strain on the heart, lowers blood pressure, and decreases the risk of developing diabetes and high cholesterol.
Quit Smoking
Smoking cessation is one of the most effective ways to reduce the risk of atherosclerosis and improve overall cardiovascular health. Smoking damages the endothelium, increases LDL cholesterol, and promotes inflammation.
Manage Blood Pressure
Keeping blood pressure within a healthy range reduces the risk of arterial damage and plaque formation. This can be achieved through lifestyle modifications and, if necessary, medications.
Control Cholesterol Levels
Monitoring and managing cholesterol levels, particularly reducing LDL cholesterol, is crucial in preventing plaque buildup. This may involve dietary changes, regular exercise, and medications like statins.
Manage Diabetes
Effective management of diabetes through diet, exercise, medication, and regular monitoring helps prevent the vascular complications that contribute to atherosclerosis.
Limit Alcohol Consumption
Excessive alcohol intake can raise blood pressure and contribute to weight gain. Limiting alcohol to moderate levels can support heart health.
Medical Interventions for Plaque Reduction
In addition to lifestyle modifications, medical interventions can help reduce plaque buildup and manage atherosclerosis. These treatments aim to lower cholesterol levels, reduce blood pressure, and prevent clot formation.
Statins
Statins are medications that lower LDL cholesterol by inhibiting the enzyme HMG-CoA reductase, which plays a crucial role in cholesterol synthesis in the liver. They are widely prescribed to reduce the risk of heart attacks and strokes.
- Benefits: Lower LDL levels, stabilize plaques, and reduce inflammation within arterial walls.
- Common Statins: Atorvastatin (Lipitor), Simvastatin (Zocor), Rosuvastatin (Crestor).
- Potential Side Effects: Muscle pain, liver enzyme elevations, and increased risk of diabetes in some individuals.
PCSK9 Inhibitors
PCSK9 inhibitors are a newer class of medications that dramatically lower LDL cholesterol levels by enhancing the liver’s ability to remove LDL from the bloodstream.
- Benefits: Significant reduction in LDL cholesterol, often used in patients who cannot achieve desired levels with statins alone.
- Examples: Alirocumab (Praluent), Evolocumab (Repatha).
- Potential Side Effects: Injection site reactions, flu-like symptoms.
Antihypertensive Medications
Medications that lower blood pressure are essential in managing hypertension, a major risk factor for atherosclerosis and heart failure.
- ACE Inhibitors: Reduce blood pressure by relaxing blood vessels. Examples include Lisinopril and Enalapril.
- ARBs: Angiotensin II receptor blockers that help relax blood vessels. Examples include Losartan and Valsartan.
- Calcium Channel Blockers: Prevent calcium from entering heart and blood vessel cells, lowering blood pressure. Examples include Amlodipine and Diltiazem.
- Diuretics: Help the body eliminate excess sodium and water, reducing blood volume. Examples include Hydrochlorothiazide and Furosemide.
Antiplatelet Agents
Antiplatelet medications prevent blood clots from forming by inhibiting platelet aggregation, thereby reducing the risk of heart attacks and strokes.
- Aspirin: Often recommended for individuals at high risk of cardiovascular events.
- Clopidogrel (Plavix): An alternative to aspirin, especially in patients with aspirin intolerance.
Advanced Medical Procedures
In cases where atherosclerosis leads to significant arterial blockage, advanced medical procedures may be necessary to restore blood flow and prevent acute cardiovascular events.
Angioplasty and Stent Placement
Angioplasty involves inflating a balloon within the narrowed artery to widen it. Often, a stent (a small mesh tube) is placed to keep the artery open.
- Benefits: Minimally invasive, quick recovery, and effective in restoring blood flow.
- Risks: Artery damage, blood clots forming in the stent, and restenosis (re-narrowing of the artery).
Coronary Artery Bypass Grafting (CABG)
CABG is a surgical procedure that creates alternative pathways for blood flow by grafting vessels from other parts of the body to bypass blocked arteries.
- Benefits: Effective for multiple arterial blockages, reduces symptoms, and improves survival rates.
- Risks: Infections, bleeding, heart rhythm problems, and complications related to anesthesia.
Endarterectomy
This surgical procedure involves removing plaque buildup directly from the inner lining of an artery to restore normal blood flow.
- Applications: Commonly performed on the carotid arteries to prevent strokes.
- Benefits: Direct removal of plaque, reducing the risk of clot formation and improving blood flow.
- Risks: Nerve damage, restenosis, and procedural complications.
Monitoring and Managing Atherosclerosis
Continuous monitoring and management are essential for individuals with atherosclerosis to prevent the progression of plaque buildup and reduce the risk of cardiovascular events.
Regular Health Check-ups
Frequent consultations with healthcare providers allow for the assessment of cardiovascular health, monitoring of cholesterol and blood pressure levels, and timely adjustments to treatment plans.
Imaging Studies
Periodic imaging studies, such as echocardiograms, stress tests, and coronary CT scans, help evaluate the extent of arterial blockage and the effectiveness of treatment interventions.
Medication Adherence
Consistently taking prescribed medications as directed is crucial for managing cholesterol levels, blood pressure, and preventing blood clots, thereby controlling plaque formation and progression.
Lifestyle Modifications
Incorporating and maintaining healthy lifestyle habits are fundamental in managing atherosclerosis:
- Balanced Diet: Focus on a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Regular Exercise: Engage in at least 150 minutes of moderate-intensity aerobic activity per week.
- Weight Management: Maintain a healthy body weight to reduce the risk of hypertension and diabetes.
- Smoking Cessation: Avoid tobacco use to prevent further arterial damage.
- Stress Reduction: Implement stress-management techniques to support overall heart health.
For an overview of heart and vascular wellness—including atherosclerosis prevention basics—see: Cardiovascular Health: The Definitive Guide to Heart and Vascular Wellness.
Conclusion
Plaque formation in arteries is a critical factor in the development of atherosclerosis, a leading cause of cardiovascular diseases such as heart attacks and strokes. Understanding the mechanisms behind plaque buildup, recognizing the risk factors, and implementing preventive measures are essential steps in combating this condition. Through a combination of lifestyle modifications, medical management, and, when necessary, surgical interventions, individuals can effectively manage arterial plaque and reduce the risk of severe cardiovascular events. Early detection and proactive management play pivotal roles in enhancing heart health and ensuring a better quality of life.